Hip Labral Tears: Everything You Need to Know About Hip Pain, Injections, Surgery, and Functional Training Solutions.
If you’re experiencing hip pain, you might be wondering if it’s a symptom of joint damage and a labral tear. Read on to learn what the science says on the correlation between pain and labral tears, how to figure out what may be causing your discomfort, and ways to work toward pain relief.

Table of Contents
- What are Hip Labral Tears?
- How do You Know if You Have a Labral Tear?
- Hip Pain and Labral Tears
- Do Hip Labral Tears Cause Hip Instability?
- What are Treatment Options for Labral Tears?
- Recap: What You Should Do if You Think You Have a Labral Tear in Your Hip
Maybe your doctor has said you have a labral tear in your hip, or maybe you’re experiencing hip pain and wondering if it’s related to a tear.
Hip pain is becoming an extremely common complaint in the age of desk work and constant sitting. It’s also becoming very common for people to get diagnosed with a hip labral tear.
In this article, I’ll take a deep look at the research around hip pain, labral tears, when to consider surgery (hardly ever), and how functional training can help. If you’re in hip pain, you’ll have a better sense of whether or not you might have a tear, and if you do, whether you should take action, and how.
But first, what is a labral tear?
What are Hip Labral Tears?
A labral tear is damage to the little cartilaginous ring around the joint. Orthopedic surgeons may tell you that this can lead to catching, clicking, and irreversible damage to the hip joint. They may tell you that when the labral cushion deteriorates, it can cause movement problems and eventually arthritis.
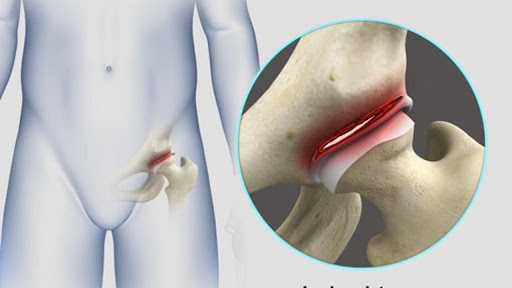
This is what a labral tear looks like.
I’ve worked with a lot of clients who have hip issues, and I have put a lot of thought and energy into understanding both the myths and facts around hip pain, hip labral tears, and other hip joint pathologies. I always want to make sure that what I’m doing with clients makes sense and won’t make things worse.
Many doctors think that less movement is the only logical prescription. That can be a pretty disempowering perspective, and it can also lead to more problems down the road.
In my experience, even if you have a labral tear, movement is the path toward better mobility and less pain, while conventional treatments for a labral tear can cause even more discomfort.
In this article I’ll explain why movement can be so helpful and why a labral tear diagnosis itself is untrustworthy and harmful to your hip health. I’ll also share what to really expect from common medical treatments for hip labral tears and what you can do to improve your hip pain and function in the long run.
How do You Know if You Have a Labral Tear?
If you’re reading this, a doctor probably told you that you have a labral tear. You probably have hip pain, and a magnetic resonance imaging (MRI) or magnetic resonance angiography (MRA) may have come back with a positive result for a labral tear.
So it’s time to stop all movement and schedule surgery, right? Not so fast.
While medical doctors will tell you that labral tears cause hip pain and movement dysfunction, the scientific literature shows a different story altogether.
In fact, there are no reliable physical tests (movement tests) that can tell you if your hip pain is from a labrum tear, and research on the effectiveness of surgery to fix hip labral tears shows surprisingly bad results.
Sounds crazy, I know. Let's jump in.
Tommy's story proves it's possible to heal your hips without surgery.
The Reliability of MRI and MRA for Diagnosing Labral Tears
Okay, so you have a scan that says you have a labral tear. Research shows that MRI and MRA have very high false positive rates, making the findings ambiguous.
A 2011 study on acetabular labral tears looked at MRI and MRA accuracy. Researchers evaluated 19 published papers that covered 881 hips. They found that MRI had a specificity of 79 percent and MRA had a specificity of 64 percent. The lower the specificity, the greater the chance you’ll be diagnosed positive, even if you’re not! Put another way, if you didn't have a labral tear, your chance of getting a false positive could be as high as 36 percent!
These two imaging strategies for diagnosing labral tears proved to be unreliable, but the study concluded that MRA is a bit better than MRI at finding tears (since it has fewer false negatives).
Another study on MRA and acetabular labral tears from 2012 found that the false positive rate could be from 25 percent to as high as 50 percent!
But physicians still have confidence in their imaging technology. Some surgeons point to this 2017 study published in the Egyptian Journal of Radiology and Nuclear Medicine which examined at the accuracy of MRI and MRA.
The authors claimed MRA was 96 percent accurate during their study in diagnosing labral tears! This is suspicious given what we have seen in other studies. So what gives?
The design of the study has a high risk of bias. It has a small sample size, no control group, and no randomization.
In fact, all 50 patients had hip pain complaints. All 50 were eager and ready for hip surgery to address their hip pain. After imaging, the surgeons cut in and confirmed or denied the presence of abnormalities.
This introduced a high risk of “assessment bias.” This is when researchers evaluate patients differently (radiographic measurement, side effects, etc.) if they already think one treatment is not as effective as another,” according to an article on study design in the journal Clinical Orthopaedics and Related Research.
In the study published in Egyptian Journal of Radiology and Nuclear Medicine, it seems no other treatment options outside of surgery were considered. Once the surgeons cut open the patients, it might follow that they were inclined and incentivized to find a justification for their preferred solution.
What's worse is that it appears the surgeons themselves interpreted the images. Their opinions were not evaluated by radiologists, so there was no independent verification of the image results.
In short, this is a study whose results cannot be trusted. The deck was stacked by surgeons to show positive results for a tool that encourages more surgeries.
Even if MRA is as accurate at detecting labral tears as the authors claim, there is an even bigger question to address: Does a hip labral tear even cause hip pain?
We’ll dive into that after we discuss physical tests (sometimes called “special tests” for hip labral tears).
The Reliability of Physical Tests for Diagnosing Labral Tears
Sometimes doctors and therapists use physical tests to determine whether your hip problems are caused by labral tears. The idea is that if you move someone’s hip joint in specific ways and you run into specific movement limitations, you can say someone has a labral tear.
A 2010 study put this idea to the test. Researchers examined the sensitivity, specificity, and accuracy of four different hip maneuvers that are supposed to tell you whether pain is from labral tears or other intra-articular sources.
All four hip tests had specificity ratings worse than a coin toss. The best specificity score was with the Stinchfield test, which looks at the relationship between hip flexor engagement and pain, and even that was accurate just 32 percent of the time. That means that positive results for labral tears on these tests have a very high risk of being false positives.
Sometimes doctors claim that using multiple tests will increase the certainty of the result. In a way, they’re right.
In this same study, combining multiple tests led to a nearly 100% guaranteed “positive” result, even if the patient didn’t have a labral tear or other hip joint pathology.
In other words, if you do multiple tests with high false positive rates on a patient with no labral tear, you have a 100% chance of a false positive.
This is crucial to understand. MRI or MRA have high false positive rates. The physical tests have extremely high false positive rates. If you use these inaccurate tools to find labral tears, you’re guaranteed to find them (even if they aren't even there!).
The bottom line? With tests this unreliable, the only way to see and confirm a labral tear is to cut into your body and look inside, but that’s not a good idea unless you’re 100 percent sure a hip labral tear is actually causing your hip pain!
And, as we’ll see later, it's impossible to tell if your hip pain is coming from a hip labrum tear.
See also : RIIPS: Why Rest, Ice, Injections, Pills, and Surgery Shouldn’t be Your Only Options
The Reliability of Anesthetic Injections for Diagnosing the Cause of Hip Pain
Often, surgeons claim hip injections are a reliable way to identify the cause of your hip pain.
The idea is that if an anesthetic injection temporarily stops the pain, you have a labrum tear. If you don't have a labrum tear, then you won't get relief from the injection.
But, again, there's no strong evidence for this belief.
In a 2008 study, the authors looked at 105 patients to see if anesthetic injections could help them identify who had pathologies like labral tears in their hips.
The researchers used patient symptoms and MRI to see if they could find a correlation between symptoms, the imaging findings, the injections, and hip joint pathology (e.g. labral tears).
The researchers considered a 50 percent reduction in pain symptoms as a positive response to an injection. If a patient got a positive response, then it meant their pain was coming from something like a labral tear (or other joint pathology).
If you're a doctor using injections to diagnose hip joint pathology, you want strong correlation between the positive response to injection and actual hip joint pathology.
This study showed very weak correlation. Only 39 percent of patients with confirmed labral tears had a positive response to the injection. 55 percent of patients with possible, unconfirmed hip labrum tears did respond to the injection.
In other words, you couldn’t tell anything from these injections. They were not better than a coin toss.
The researchers checked to see if other physical tests could help identify tears, but they found no correlation between those test results, injections, and the presence of a hip labral tear.
Now there is one more symptom that doctors often point to for hip labral tears that we haven't yet discussed.
So let's look at popping, snapping, clicking, and clunking in your hips and what it might have to do with hip labrum tears.
Watch this case study of a medical professional with hip pain resolving her discomfort with functional training, not surgery or injections:
Joint Popping, Snapping, and Clicking and Labral Tears
Maybe you’ve heard your hip pop or snap and are worried that sound is a symptom or sign of a labral tear.
This is a belief that is echoed all over the internet and is extremely common to hear from doctors.
For many reasons, it seems unlikely that popping, snapping, and clicking sounds are indicators of a labral tear.
The top reason this is unlikely is that the labrum itself is not stiff enough to catch on anything to make a loud clicking sound. The labrum is like a small cushion in your joint.
Imagine sitting on a pillow and trying to make a snapping sound by rubbing your butt on it. No matter how hard you rub, you will not get a clicking, snapping, or popping sound. This is something a six-year-old can reason out.
To get a snap, pop, clunk, or crack, you need stiffer substances to rub against each other. What do we have around our hip joints that is stiff enough to make snaps, pops, clunks, and cracks?
We have bone. We have tendons (which are the stiffest portions of muscle as they connect to bone). Tendons rubbing against each other or against bone could conceivably create those pops, cracks, thunks, and clunks.
That's my theory. And while there have been no studies to determine if this theory is true, it at least passes the basic plausibility test better than the orthopedist's fantasy of a soft piece of tissue somehow making clicking noises.
Watch this video for a visual breakdown:
In short, there is currently no way to reliably determine that a person’s hip pain is coming from a hip labral tear. MRIs and MRAs aren't reliable. Physical tests aren't reliable. Sound effects aren't reliable either unless you're willing to suspend your critical thinking skills entirely.
That might make you feel a little lost. If the doctor's box of tests is totally useless, how will you fix the hip pain caused by your hip labral tear?
First, remember that you actually don't know that your pain is from the labral tear (since there is no test to determine it).
Second, a labral tear is likely not even the cause of your hip pain. Let's dive into the research.
Hip Pain and Labral Tears
A lot of the information you find on the internet from reputable medical sources claims that hip labral tears are associated with hip pain.
At this point in the article, you may not be surprised to learn that many studies have shown little to no correlation between hip labral tears and pain.
These MRI studies looked at the hip health of asymptomatic people (meaning people without hip complaints).
In one study in 1998, researchers examined 52 asymptomatic hips to tease out the relationship between hip labral tears and hip pain.
They found that the majority of study subjects had some level of labral tear or other hip lesion.
In a similar study in 2012, a whopping 85 percent of asymptomatic volunteers had hip labral tears.
In 2015, another study revealed that 39 percent of asymptomatic people had hip labral tears. The authors concluded: “Given the high prevalence of labral pathology in the asymptomatic population, it is important to confirm that a patient’s symptoms are due to the demonstrated abnormalities when considering surgery.”
But remember: there are no reliable tests to confirm your hip pain is from a labral tear.
In short, hip labral tears are very common in people without hip pain. Just because you have hip pain and a labrum tear on an MRI or MRA does NOT prove the hip labral tear is causing your hip pain!
The authors of this 1998 paper point out explicitly that labral tears in imaging "are especially frequent and may represent asymptomatic lesions or normal variations."
So it's best to think of your hip labrum tear as a normal variation and address the organs around your hip that surgeons ignore. These organs help you stabilize and move your hip.
And while we're talking stability, you might still be wondering if hip labral tears affect the stability of your hip joint...
Do Hip Labral Tears Cause Hip Instability?

Nobody likes instability. Credit: Stock Unlimited
For years, surgeons have believed that labral tears cause instability in the hip joint. This instability supposedly can only be “fixed” by either cutting out or securing loose labrum tissue via surgery.
In 2011 study, a group of researchers tested the idea that a labral tear would lead to joint instability by using finely tuned instruments and hip joints from human cadavers. They created labral tears and then measured the effect on joint stability.
Their findings were almost the exact opposite of what they expected. They tested circumferential tears and radial tears (basically different orientations of tears) to see if it mattered. They also tested hip joint stability after labrectomies (removing torn pieces of the labrum).
Their results?
Even big tears in the labrum did not result in loss of stability in the hip joint.
There was no significant difference in stability after a radial tear or a one-centimeter partial labrectomy, compared with an intact labrum.
On the other hand, a two-centimeter partial labrectomy, or removal of parts of the labrum, significantly decreased stability. Read that again. A once-popular medical treatment for hip labral tears clearly worsened the hip stability.
The authors' conclusion: Even big hip labral tears do not cause instability in the hip joint. Removing pieces of the labrum does.
At this point, it should be clear that the medical approach to labral tears is horribly out of whack with research evidence. The tests don't work. The images are wildly unreliable and overinterpreted. The theories about pain, clicking, locking, and hip labral tears are not based on evidence.
So what about treating hip labral tears? Surely there's good evidence there?
What Are the Treatment Options for Labral Tears?
If you have been diagnosed with a labral tear, your doctor may have recommended surgery. I’m here to present the science behind that option, as well as offer a different solution.
Movement and functional training can help you relieve hip pain, restore range of motion, and get your life back. By properly training the muscles around your hip joint, you can accomplish far more than the empty promises of labral tear surgeries.
Do Surgeries for Hip Labral Tears Work?
When you do research on surgery for hip labral tears, you’ll find the vast majority of medical information sites tell you that this is the only option for healing.
One of the most popular treatments for hip labral tears in the last decade has been labral debridement (or labrectomy). This is when a surgeon goes into your hip and cuts away the “loose” bits of your labrum. As noted earlier, removing pieces of labrum actually increases instability.
So, you won't be surprised that a 2014 study showed dismal results for labral debridements/labrectomies. The researchers found that nearly half of the 57 patients who had undergone labral debridement ended up with poor results.
In a stunning display of pro-surgery bias, the study authors proposed that the reason patients got bad results from the labrectomies is that the surgeons should have also cut away bone.
It’s like saying, “We tried to fix your flat tire by removing a nail. It didn't work. So we also need to replace the axle and the fender."
See also : Why you DON’T Need Orthopedic Surgery for Joint Pain
The other surgical option for a hip labral tear is refixation, where the “damaged” labrum pieces are reattached.
This 2009 study looked at the difference between debridement/labrectomy and refixation. Refixation had much better outcomes than debridement in this retrospective study. But because it was a retrospective study and not a prospective study, its conclusions should not be counted on as gospel truth.
It's also important to take a step back and consider the idea and mechanics of the refixation surgery. Does it seem sensible and plausible?
Refixation involves puncturing the labrum and the pelvis to create attachment points to affix the labrum to the acetabulum. Does adding more damage to the labrum and to the pelvis make any sense? Would you fix a flat tire by punching holes around the original hole and stitching a patch on the original hole?
This wouldn't pass a kindergartner's logic test.
Many orthopedic surgeries have been used for decades without any serious scientific investigation. With hip labral tears, there have been few comparisons between the surgical approach to more conservative approaches and no placebo-controlled studies.
One study, published in 2021, compared surgery with physical therapy for labral tears. Researchers ran an allegedly randomized controlled trial and concluded that surgery was better than physical therapy after a 12-month follow-up.
However, when you dig deep into this study (Hip Arthroscopy Versus Physical Therapy for the Treatment of Symptomatic Acetabular Labral Tears in Patients Older Than 40 Years: A Randomized Controlled Trial), you see that it's plagued with methodological problems and massive bias.
First of all, the patients were recruited through a hip surgery clinic. This means the patients were strongly interested in surgery before the trial even started. Once recruited into the study, they were required to go through a "conservative treatment" period.
They were told not to do anything to aggravate their hip pain and not to do flexibility or strength training. They were told to follow a poorly designed physical therapy protocol. Some also received hip joint injections to numb the pain. If the patients didn't improve from this misguided conservative care protocol after a few months, they were allowed to participate in the trial and be randomized to more physical therapy or surgery.
Think about this. You have hip pain and go to a hip surgeon's clinic to get a surgery you think will help. The surgeon tells you to do essentially nothing and hope it gets better for a few months. But he and his staff also tell you that doing nothing won't fix anything, because the only thing that can fix you is surgery.
When you come back, you're assigned to a surgery or non-surgery group. If you just spent a few months getting no results and the doctor's team keeps telling you that the only way to fix your problem is surgery, which group are you going to want to get into? The bias for surgery is built in before the trial even begins...
If assigned to surgery, the patient got surgery. If not, the patient was assigned to more pointless and poorly designed physical therapy.
As I mentioned, the physical therapy protocol disallowed any serious flexibility or targeted strength training. It also included thorough "patient education" to ensure that patients believed they had a bone problem that could not be fixed with exercise. Furthermore, physical therapists and doctors in the study reiterated that any movement that was uncomfortable in the hips was to be avoided to prevent further hip "damage."
And here's the kicker.
They told patients if they didn't see progress in physical therapy after a few months, they could switch to the surgery group! Unsurprisingly, a whopping 63% of the patients in the "physical therapy" group ended up getting surgery halfway through the study.
In any independent and dispassionate analysis, this would completely disqualify this study as a well-designed randomized controlled trial.
If you're going to compare two treatments for two groups, you have to keep the groups separate to draw useful conclusions. You also shouldn't be telling the study participants that one of the treatments has no hope of helping and that they can switch to the better treatment! This is "assessment bias" at its absolute worst.
To rescue this garbage from the dustbin, the researchers employed multiple statistical analysis tricks and highly biased scoring systems to claim that surgery came out significantly ahead of physical therapy.
In reality, the scoring systems they used, the iHot-33 and the Harris Hip Score, showed only minor differences between surgery and physical therapy that can be explained by the bias within the scoring systems themselves.
Watch this video for a thorough, detailed breakdown of this terrible study and the scoring systems involved.
So, to recap: Surgery may sound promising initially when your doctor presents it as an option, but many people who get surgery actually discover that their pain doesn’t go away. Some discover their range of motion is worse.
Based on my experience as a functional trainer who has seen hundreds of clients with hip pain, pre- and post-surgery, I don’t recommend surgery as a first step.
Here’s why: Surgical treatments for hip, back, shoulder, and knee pain may have been invented by well-intentioned surgeons, but rigorous scientific investigation routinely debunks orthopedic surgeries and other conventional Western treatments for joint pain.
Conventional medicine emphasizes quick short-term “fixes" based on narrowly defined criteria for success that don't align with a patient's desires. Financial incentives from insurance companies for expensive treatments keep scientifically debunked surgeries raging.
And there can be a total mismatch of what "success" means to a patient and what it means to a surgeon. For patients, success is measured by the ability to return to daily life and any specific athletic endeavors that they love. It's not just about surviving the surgery with minimal scarring.
I've spoken with many people who have had hip surgery to fix a hip labrum tear. A large number of them were told they should never go back to high-impact, high-intensity activities after surgery. If their pain is improved but they do not regain full activity levels, is that success? It is to the surgeon.
In addition, surgery comes with a whole host of recovery issues. The required period of rest after surgery leads to atrophy. That leads to movement issues and more pain. If you don't use your muscles, you lose them. And the more you lose, the worse you'll feel.
Here’s another case study, of someone with hip pain who found relief through functional training, NOT surgery:
Functional Training for Hip Mobility and Hip Pain
If you’re experiencing pain or reduced range of motion in your hips, retraining your hip muscles can save you thousands of dollars, months of bed rest, and an unpredictable risk of bad outcomes.
And while the process is not a quick fix, it’s a solution that gives you the power to relievehip pain and increase your ability to enjoy all the activities you love, even the high-impact, high-intensity ones!
As a functional trainer, I want to keep you moving, and am always looking for ways to improve your range of motion, comfort level, and overall athletic competency.
Doctors may tell you your best hope is to rest and pray.
But rest only leads to atrophy and decay.
See also : How to Identify Muscle Imbalances and Muscle Dysfunction
I’ve seen people with severe hip pain regain full function of their hips without surgery. These are cases that prove the medical perspective is at least incomplete if not completely wrong.
I’ve also seen people get hip surgeries to repair labral tears, only to have the pain remain the same or get worse.
Proper retraining of the muscles around the hip will actually get rid of the pain and restore function to the hip in a way that surgery doesn’t!
Here’s another client story, from someone who needed to recover from hip pain AFTER surgery:
Recap: What You Should Do if You Think You Have a Labral Tear in Your Hip
First, I'm not a doctor and this isn't medical advice. This is extremely non-medical advice.
If you have been told you have a labral tear or you THINK you have a labral, think about these major points:
- Is there any way to know whether you have a labral tear? Without surgery, there’s no definitive way to know.
- Is there any way to know that the labral tear is actually causing your hip pain? Based on the research, NO! People with hip pain in research studies often don’t have labral tears, and vice versa. Remember: Just because a doctor believes something is true does not actually mean it's true.
- What’s the likelihood that surgery will fully fix your hip pain? Read papers like the ones you find here so you understand the history of surgeries to “cure” pain. A surgeon saying, “surgery is guaranteed to fix your hip pain,” sounds good, but the research doesn’t back it up.
Tthe most important factor for getting out of hip pain is training your hip muscles to work properly - gradually and carefully. It doesn't matter if you've already had surgery that failed or you're thinking of getting surgery.
That is a process that requires time, learning, and patience. I strongly encourage people to acknowledge their fears and anxieties around labral tears, recognize that there’s very little evidence that labral tears actually are the definitive cause of pain, and focus on the muscles around the hips.
In other words, ATM: Always Think Muscles.
Your muscles move your bones. They are the organs responsible for moving your body parts properly. If bones collide in the wrong way, it's because of how your muscles are moving them.
You can improve control of your muscles. You can retrain muscles with stretching, self-massage, and carefully executed exercises.
See also: How to Fix Muscle Imbalances and Muscle Dysfunction
Here is what I suggest, if you’re experiencing hip pain or think you have a labral tear:
- Find a trainer, coach, or physiotherapist who can coach you to move with good form in new ranges of motion. If the professional you choose works from a cookie cutter template, find a new one. Please don’t jump into high-intensity interval training or some kind of boot camp, group class, or Crossfit situation until you’ve worked with a professional.
- Learn how to stretch properly (not aggressively). Learn how to get stronger. At first you may over-interpret some sensations as threatening, but with practice, you’ll learn what your sensations mean (and they aren’t always warning signs that something is horribly wrong). Get curious. Strive for strength at every length.
- Always think muscles! Learn more about how and why pain you feel in your joints is likely really due to muscle imbalance and dysfunction.
- Identify muscles that are weak and build strength.
- Identify positions you find difficult and carefully work to make those positions more comfortable (by training the muscles there).
- Don’t stress! Labral tears are not related to symptoms, thus there is nothing specific about them that you need to worry about. Hip pain and dysfunction are related to muscle function and are far more important than a bogus diagnosis.
If you are experiencing hip pain, read my article on muscle dysfunction: ATM Theory: Your Joint Pain May Actually be Muscle Pain
Curious about the orthopedic surgery industry? Read: Why you DON’T Need Orthopedic Surgery for Joint Pain


